The post is a response to a conversation I have both online and in my clinical practice. It revolves around the difficulty in assessing the bodyfatness of a child. Specifically I see online a post similar to “Look at this picture of my darling child, can you believe that his/her doctor said they were obese?!!?” In my clinical practice it revolves around me trying to discuss the family habits in relationship to a child that I have concerns about (often in relationship to BMI).
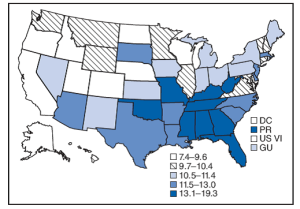
I’ll begin with a basic explanation of some data gathered in most medical practices. In medical practice we often gather height and weight at an office visit. These numbers can be graphed on a chart that compares them to a standarized set of “normal ranges”. These normal range in the US are most commonly drawn from the CDC growth charts which come out of a large range of children’s data drawn from two survey’s done between 1963-1965 and 1988-1994. So the first important point I’ll make is that most of this data for the comparison groups was gathered prior to the large increase in childhood obesity that we’ve seen in the Western world. So a child, for example, that is “80% for weight”- probably isn’t 80% for weight compared to youth around them right now (because average weight of children has increased)- but 80% compared to children in that historical data set.
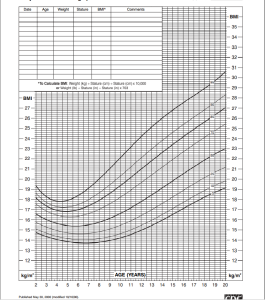
So often we will graph a child’s height and weight relative to that data set, but we will also then often graph two other data sets against similar “growth charts”- one for height/weight ratio and one for BMI. In my mind these are just two sides of the same coin, but because of the way BMI is calculated the shape of the graph is very different (because BMI = Weight in pounds divided by height in inches squared multiplied by 703). Because the height is squared the graph is somewhat less linear. At the end of the day the percentages (meaning where a child appears on the graph relative to that historical “normal range”) will be roughly the same. For the purposes of the rest of this discussion I’ll focus on BMI, in part because BMI often gets a bad reputation in and out of medicine (partially deserved and partially inaccurately). Here is the graph for the BMI nomogram from the CDC.
So this is a graph of BMI on the Y axis and age 2-20 on the X axis. The first thing you see is that sometime after age 2 is when kids normally “get too skinny”. I often see kids that parents bring in at age 3-5 “because they are getting too skinny”, but you can see on the graph that is pretty normal. This is called adiposity rebound- toddlers grow more in height then they do in weight and then at some point they start gaining more mass relative to height and the BMI naturally increases. My wife got sad over the last year as our 2 year old “lost her baby fat” and transitioned from that normal chubbier toddler appearance to the thinner 3 year old. The graph shows that that’s normal and even the heavier kids historically had some degree of that. The thinner kids often have a longer period of staying thinner.
Two more basic definitions: in medicine the normal range is considered to be 5-85 percentile when compared to this historical data set. Overweight is 85-95 percentile and Obese by pediatric BMI is considered over 95 percentile. This is somewhat different then how we do things in adults where we have ranges of BMI that set those same values, but as you can see above a 3 year old with a BMI of 20 (which is quite thin in an adult) would be off the chart heavy. It’s too complex to set a normal BMI range for each age group so by convention we set the normal ranges by the percentile on that graph.
A note on BMI. In a recent discussion I was involved in I heard several people disparage BMI as not being accurate and “should be thrown out”. The issue with that sentiment is that it’s just not supported by science. That said, you have to have an understanding of what BMI does. BMI estimates relative body fat for populations reasonably well. Two people with the same BMI can have very different body fat %, but in-total, over large numbers of people, it does a reasonably good job. Part of that is there is a limit of how much lean mass a body can make without the use of steroids to increase mass. So at a certain point (probably somewhere over BMI 30)- if there’s no steroid use it means that excess weight is almost certainly fat.
What BMI doesn’t really do is accurately assess the health status of an individual patient. I myself have real question about what the value of the “overweight range” is on the BMI scale for both kids and adults. Many athletic people have BMI in the overweight range. There was a controversial recent study that showed people in the overweight range died less often then those in the normal weight range, so I do think there’s reason to question what “overweight” by BMI means. I do however think that (in adults) you’d have trouble finding anyone that wouldn’t argue that obese by BMI (especially grade 2 obesity- BMI over 35) correlates very closely with increased risk of many medical problems.
There are several factors that also need to be considered when looking at BMI (from the CDC website):
How good is BMI as an indicator of body fatness?
The correlation between the BMI and body fatness is fairly strong1,2,3,7, but even if 2 people have the same BMI, their level of body fatness may differ12. In general,
- At the same BMI, women tend to have more body fat than men.
- At the same BMI, Blacks have less body fat than do Whites13,14, and Asians have more body fat than do Whites15
- At the same BMI, older people, on average, tend to have more body fat than younger adults.
- At the same BMI, athletes have less body fat than do non-athletes.
The accuracy of BMI as an indicator of body fatness also appears to be higher in persons with higher levels of BMI and body fatness16. While, a person with a very high BMI (e.g., 35 kg/m2) is very likely to have high body fat, a relatively high BMI can be the results of either high body fat or high lean body mass (muscle and bone). A trained healthcare provider should perform appropriate health assessments in order to evaluate an individual’s health status and risks.
So what about kids? Well the thing is that kids (because of the difference in hormones) have even more limit on how much lean mass they can truly produce. This study shows that about 85% of kids in other Obese range (on the BMI chart above) are in excess of what is considered the normal range of body fat. So yeah, it’s not all, but 85% of those found to be obese (by BMI)- truly are obese as defined by above normal body fat percentages.
So again, we don’t find that BMI is perfect for defining risk in one single kid, but it does a good job of assessing those that are potentially at risk.
“But how can that be doctor, my child looks perfectly healthy and normal, he can’t be over-fat!”
So lets run some numbers to see how tricky this can be. Without getting too complex, let’s look at an imaginary 10 year old child that is average height (56 inches). A weight of 100 pounds would give him a BMI of 22.4 and put him above the 95% on the graph above. That child is obese by BMI (and therefore an 85% chance that the child has excess body fat compared to what is considered normal). If that same child weighed just two pounds less at 98 pounds- he would be BMI 22.0 and in the overweight range (and considerably less chance of being over-fat compared to normals). Likewise if the child weighed 90 pounds he would be at a BMI considered in the normal range (5 to 85 percentile).
I don’t know about you but I’m not sure I would *by visual inspection* be able to identify a kid that had 2 pounds of extra fat on them (and therefore overfat compared to the kid that had 2 pounds less fat).
Let’s look at this another way: mathematically without BMI. Normal body fat % for a ten year old is something like 13-23% and obese is over 27%. That’s a difference in a 100 pound kid of just 4 pounds! I really don’t think my ability to visual assess bodyfatness is accurate to 4%.
So what do you do when your kid is obese by BMI? Heck, what do you do if you are obese and over-fat and want to try to change that? Examine your families habits. Take a hard look at things like “Are we eating enough fruit and vegetables?” “How much screen time a day is my child getting?” “How much sugary beverages is my child drinking per day or week?”
My office has been giving a hand out on the 5-2-1-0.
5 servings of fruits and vegetables
2 hours or less of screen time per day
1 hour of physical activity per day
0 sweet or sugary beverages per day.
I think that’s a good starting point both healthy habits in anyone frankly. I’d also add “looking at how much sleep we are getting” and for most families my advice is “get more”. Most kids need 10+ hours of sleep and we are not good at getting that in the Western world and that is often tied to the screen time.